When anti-inflammatory medications don’t work, cortisone injections may almost seem like a gift from heaven. They may appear to be the quickest treatment option for inflammation and pain relief.
Sometimes, though, the injection process may not go according to plan. For instance, a cortisone shot might accidentally hit a nerve. What happens afterward? What does it feel like? Should you do something about it or call for help?
What Happens if a Steroid Injection Hits a Nerve?
If a steroid injection hits a nerve, the affected nerve may become injured and damaged. This may result in:
- Immediate burning pain, and
- A potential loss of feeling or function in the affected area.
Most of the time, the damage is minor and heals quickly. However, the recovery process might take much longer if the nerve is completely disrupted.
Luckily, the chances of severe damage due to steroid injections are very low in developed countries.
Steroid injections, such as cortisone shots, are generally safe. They’re used for pain and inflammation relief in different body parts. An ideal cortisone shot procedure is quick and causes little to no pain, and this is also the case for most people.
Is Nerve Damage a Side Effect of a Cortisone Shot?
Nerve damage is considered more of a complication than a side effect of a cortisone shot.
As mentioned, the injection procedure may go awry, and the shot may accidentally injure an unlucky nerve. Let’s see what follows.
What Are the Symptoms of an Injection Hitting a Nerve?
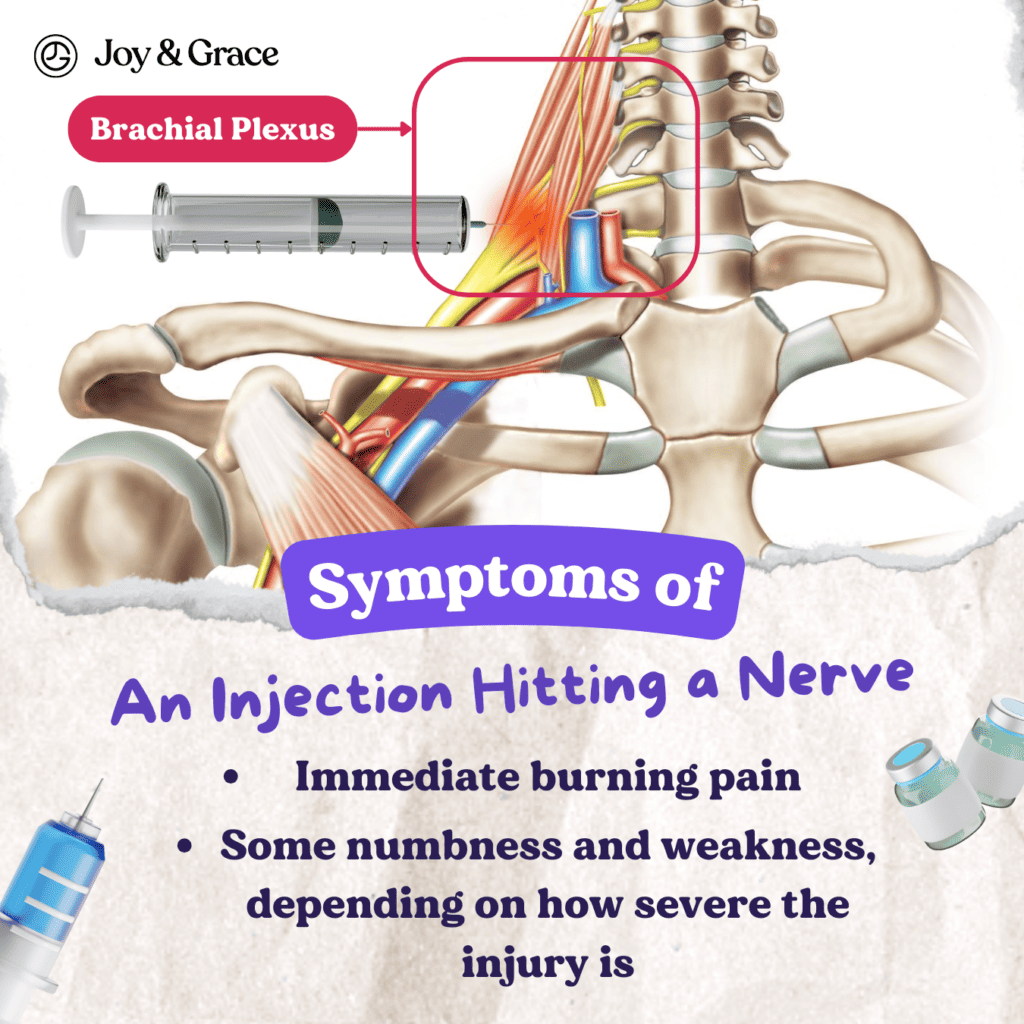
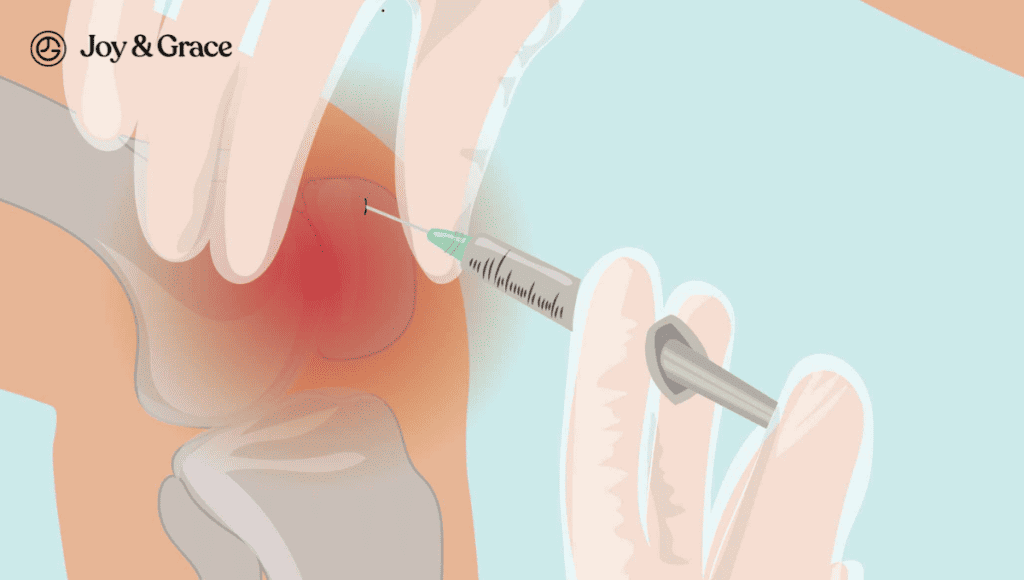
An injection hitting the nerve in this area may cause symptoms such as:
- Immediate burning pain, and
- Some numbness and weakness, depending on how severe the injury is.
That said, nerve damage from an injection hitting a nerve may manifest in various forms. For instance, depending on the injection site, a cortisone shot may hit a single nerve or a group of nerves.
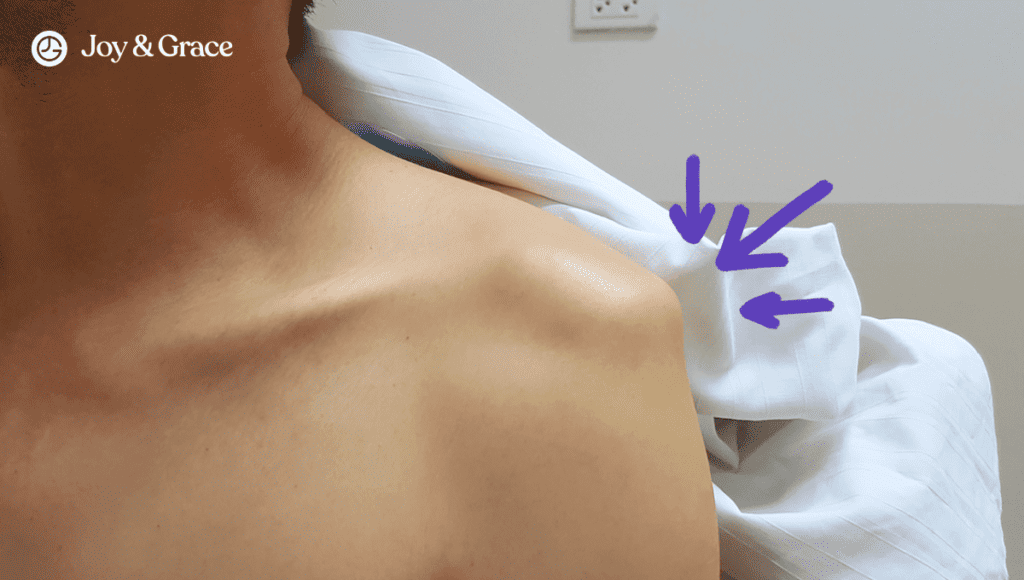
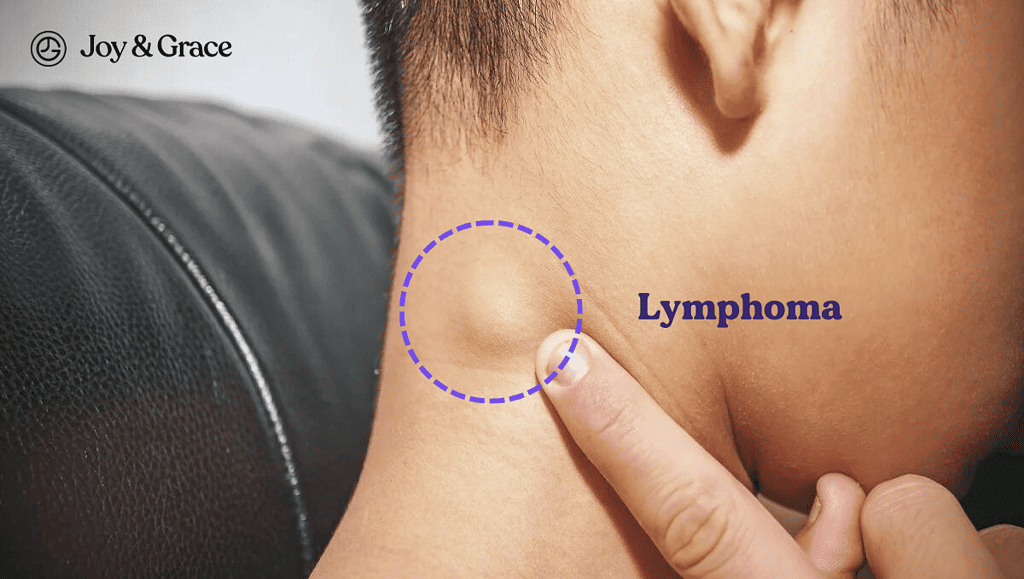
If the injection hits a group of nerves, it will affect a broader area. This can be the case with a brachial plexus injury.
The brachial plexus is a network of nerves that begins at the root of the neck and spreads toward the length of the upper limbs. A wrongly administered shoulder or neck injection might affect nerves supplying the neck, shoulder, and arm muscles.
Similarly, a spinal injection can also affect the function of a nerve bundle. If a spinal injection goes wrong, it may lead to serious consequences, such as:
- Paralysis of one or both legs
- Loss of bowel control
- Loss of urinary bladder control
- A constant strange feeling that spreads in various body areas
In other instances, a single nerve may be affected, as with median nerve injuries in carpal tunnel injections.
In such a case, symptoms are localized in a small area that the nerve supplies and include the following:
- Neuropathic pain (Sharp, shooting, or burning pain)
- Numbness (Loss of sensation)
- Tingling or prickling. This gives the impression that pins and needles are prickling your skin.
- Muscle weakness and wasting
- Changes in the way you perceive pain
You should know that pain at the injection site is normal for a few days after you receive the injection.
Simply taking a pain reliever like Tylenol and applying an ice pack can provide relief.
But if the pain goes along with the other listed symptoms, you might be dealing with some sort of nerve damage.
How Long Do Side Effects Last if a Nerve is Hit?
Permanent damage after a cortisone shot hits a nerve is very rare. Mild single-nerve injuries typically recover in a few days or weeks.
Recovery from the potential side effects depends on how severe the nerve injury is.
Most people take a few days to a few weeks to fully recover from mild single-nerve injuries. For more severe damage, full recovery is questionable. It may take months or years for the nerve function to return. In these cases, surgical correction within six months of the injury might be necessary to improve recovery.
According to studies, the incidence of nerve injury from injections ranges from 1.5 to 15%. The percentages are higher in developing countries.
To ensure proper recovery, your healthcare provider will first identify the location and degree of nerve damage. They achieve this by applying any of the following diagnostic tests:
- Nerve conduction studies
- MRI
- CT scan
Nerve damage from cortisone shots may be treated by incorporating the following methods:
- Medications. Your doctor may prescribe painkillers (such as Tylenol) or medicines that typically treat epilepsy and depression. The latter may be helpful as they interfere with how pain impulses are transmitted.
- Physical therapy and exercise. Physical activities are necessary to maintain muscle strength and mobility.
- Rest. Rest is essential to achieving full recovery. Recovering from nerve damage takes time and patience. The outcomes for mild nerve injuries are excellent.
Why Am I in More Pain After a Cortisone Shot?

A cortisone shot increasing the pain can be disappointing.
However, luckily, a transient increase in pain after a cortisone shot is entirely normal in most cases. As we also mentioned earlier, temporary or transient pain at the injection site can be normal for a few days after receiving the injection.
On the other hand, sustained pain suggests the possibility of nerve damage.
Damage to the nerve from a cortisone shot activates pain receptors and changes how the nerve fires impulses to the brain. The changed impulse transmissions are carried to the brain perceived as pain.
How Do I Know if I Hit a Nerve During an Injection? What Does Nerve Damage From an Injection Feel Like?
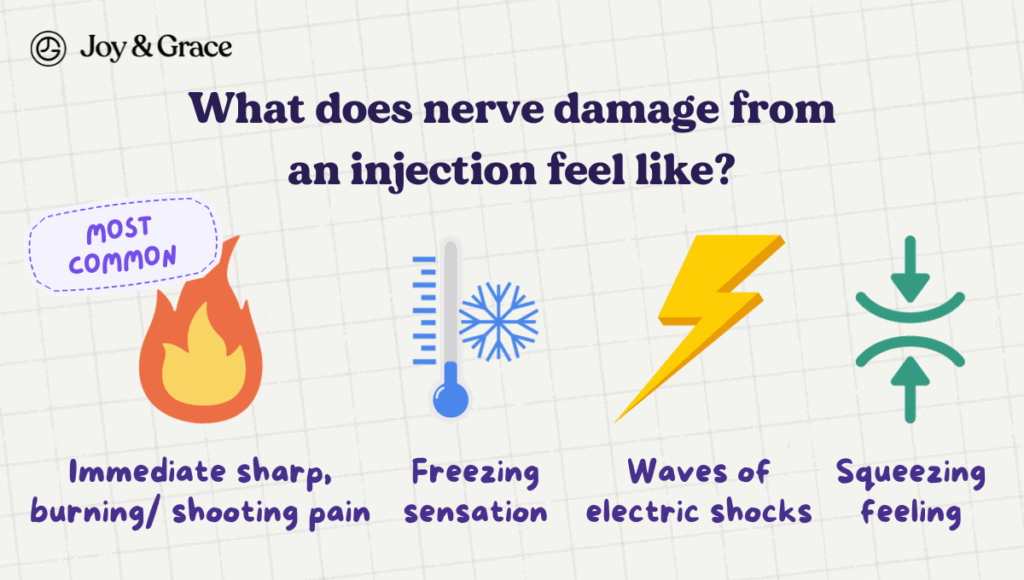
The pain due to a nerve injury is most commonly described as:
- An immediate sharp, burning, or shooting pain that may appear with other neurological symptoms like weakness and numbness.
It may also sometimes feel like:
- A freezing sensation,
- “Waves of electric shocks,” or
- A squeezing feeling.
Regarding duration, nerve damage pain can be constant or appear spontaneously in bouts.
This kind of pain that you feel after nerve damage from an injection is considered neuropathic (nerve-related).
“Neuropathic” means the pain stems from a disturbance of function in one or several nerves.
The intensity of the pain may also vary. Some people naturally have a higher pain threshold. This means they may tolerate more pain than others.
On the contrary, people with lower pain thresholds are more sensitive to pain. They may experience more pronounced symptoms.
What Nerves Are Most at Risk From Cortisone Injections?
Cortisone injections pose a higher risk to certain nerves located in vulnerable areas of the body.
The nerves most commonly damaged by cortisone shots include the following:
- Sciatic nerve (from injections in the gluteus muscle in the buttock)
- Radial nerve (from injections in the deltoid muscle in the shoulder)
- Axillary nerve (from injections in the deltoid muscle in the shoulder)
- Median nerve (from injections in the wrist or carpal tunnel)
Additionally, intramuscular injections are associated with a higher incidence of nerve injury, especially in developing countries.
What Does Cortisone Do to the Nerve?
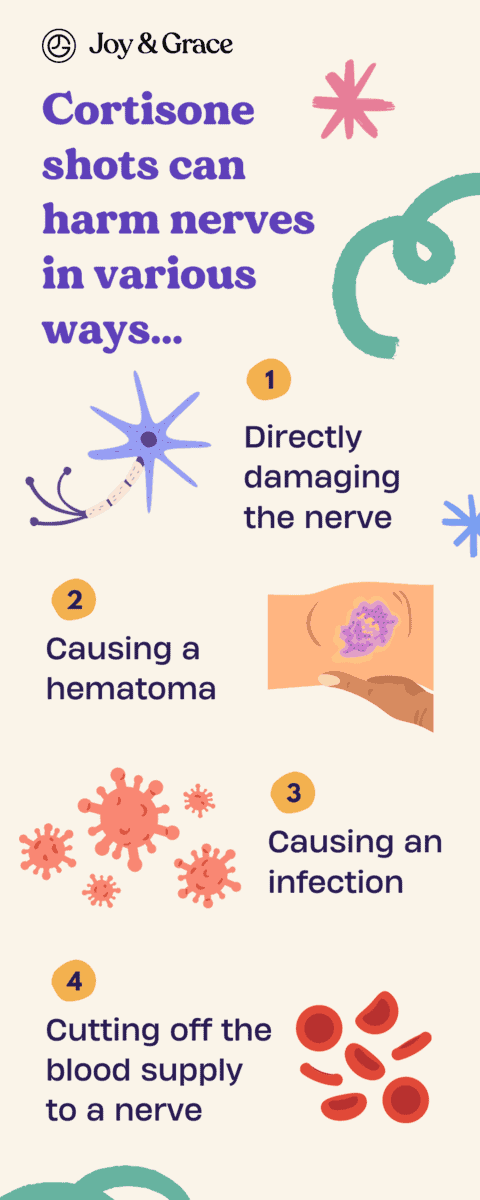
Cortisone shots can harm nerves in various ways, besides direct impact.
Let’s take epidural injections as an example. Epidural steroid injections enter the epidural space of the spine to relieve back pain. They may result in nerve injuries by:
- Directly damaging the nerve. We’ve been talking about this one throughout the article. The needle or catheter used to give the shot may compress a nerve, a group of nerves, or the spinal cord. Nerve damage is classified into five categories based on severity. A first-degree injury is like a small nerve issue. In second and third-degree injuries, some nerve fibers are cut. In a fourth-degree injury, the nerve membranes are damaged along with the nerve. A fifth-degree injury means the nerve is completely cut along with its coverings.
- Causing a hematoma. A hematoma is a collection of blood that collects under the skin after a blood vessel injury. Small hematomas are usually harmless. If the injury is more severe, more blood may escape the vessels, causing larger hematomas. Large hematomas may compress and damage a nerve, resulting in pain. By affecting blood circulation, they may also cause delayed nerve damage symptoms.
- Causing an infection. Infections may develop near the injection site if sanitary precautions are not followed. Infections may cause inflammation and abscess formation. As a result, nerves and other nearby structures may get damaged, causing noticeable symptoms. Infections should be treated with antibiotics, as they may spread and lead to dangerous complications.
- Cutting off the blood supply to a nerve. Your blood pressure may drop during certain injections, such as spinal injections. With lower blood pressure, there’s less blood available to supply the nerves. This may lead to nerve damage from a lack of blood supply.
- Administering the wrong drug. In extremely rare cases, your doctor might make the mistake of giving you the wrong drug (instead of cortisone). This drug may be toxic to nerves, thereby hurting them.
So, why do these accidents during injections occur in the first place? Let’s see below.
The Injection Needle is Incorrectly Placed
Steroid injections may be injected into various body sites. The injection site may be any of the following:
- A joint (intra-articular injection)
- A muscle (intra-muscular injection),
- The spinal cord (epidural injection), or
- The blood (intravenous injection).
The odds of nerve injury increase when the needle is placed incorrectly or at the wrong site. Thus, it’s crucial to specify the right type of injection, its target site, and its placement above the skin before performing the shot.
How Do Doctors Prepare an Injection?
To ensure the injection process goes smoothly, professionals use a set of rules. For example, they first make sure they’re using the right needle size by:
- Picking the right length and gauge of the needle needed to reach the correct tissue layer. A short needle might not reach further than the fat layer under the skin, while an unnecessarily long needle might damage the nerves, bones, and blood vessels deep inside.
- Taking into account various factors, such as:
- The patient’s age, sex, weight, muscle size, and fat percentage
- The number and recommended route of giving the injection
- The volume and thickness of the injected material
After picking the correct needle, doctors must decide on the precise injection area. This process is called landmarking. Let’s take an intramuscular injection as an example to explain landmarking:
- What Happens if a Steroid Injection Hits a NerveThe whole area surrounding the injection site is exposed.
- The injection is given in the central and thickest portion of the muscle.
- Doctors use different anatomical structures, such as bones, to determine the injection sweet spot.
- Doctors avoid areas with bruises, inflammation, swelling, tenderness, or masses. Contrary to popular belief, a tattoo on the injection site is not an obstacle.
- If the first muscle is weak or small, another muscle can replace it as the injection site.
Different People Have Different Body Anatomies
The fact that we, as humans, have almost the same basic body composition doesn’t mean our bodies are exactly the same. Anatomic variations exist!
This means a nerve may branch at different locations in different people. Even millimetric differences matter! Hence, healthcare professionals must consider this fact before giving injections. They must strive to be as precise as possible.
To increase precision, doctors may choose to give steroid injections with the help of ultrasound imaging. Ultrasound-guided injections provide real-time needle tracking. This means they visualize the needle from the moment it enters the body until it reaches its target site.
The Healthcare Professional Lacks Experience, Skill, or Concentration

Prior to administering a steroid injection to a patient, doctors must ensure they’re prepared and focused. Mistakes that occur due to a lack of preparation or focus are avoidable and unnecessary. Thankfully, they are also very rare.
To avoid affecting a nerve when giving a cortisone shot:
- Only experienced healthcare professionals should administer them.
- The patient should cooperate with the doctors and listen to their advice.
- The patient should stop taking any anti-coagulant (blood thinners, such as aspirin) a few days before to prevent bleeding.
- Sterile conditions are necessary (to avoid contamination and infection).
- The patient’s condition should be monitored after receiving the injection.
Was the Steroid Injection Really at Fault?
We now know that a mistake during an injection can be an unfortunate cause of nerve damage. But it’s not the only vile culprit! There are other ways nerve damage may happen, as follows:
- Surgery procedures. Some locations inside the body are difficult to reach. In difficult operations, nerve damage is a minor, plausible side effect. A 2014 study shows that 94% of accidental nerve injuries happen during surgical procedures. Your surgeon will naturally inform you of this possibility beforehand.
- Keeping a certain position during an operation. Certain body positions may put long-lasting pressure on nerves and injure them.
- Using tourniquets. Tourniquets are bands that apply pressure to body areas to reduce blood loss. This applied pressure may also compress and damage nerves.
- Post-operation swelling. Even though swelling is normal after a surgical operation, it may cause pain by compressing a nerve.
- Medical conditions (like diabetes or blood vessel diseases). Some pre-existing conditions can narrow blood vessels. Narrowing the vessels limits blood supply and increases the chances of nerve injuries.
How Often Can I Get a Cortisone Shot?
Too many cortisone shots at the same site can cause more harm than good. For example, if intra-articular injections are repeatedly given in the same joint, nearby joint tissues (such as cartilage) may break down. Corticosteroid injections can also weaken the skin at the injection site and thin the soft tissue underneath.
Thus, it's best not to have more than three or four cortisone shots per year for any body region.
What Are the Other Cortisone Shot Side Effects?
Nerve damage happens in less than 1% of cortisone shot procedures. Other side effects are uncommon as well. They depend on the type of injection and may include the following:
- Pain and discomfort. Consider taking Tylenol or an NSAID like Ibuprofen.
- Bruising or a collection of blood under the skin (a hematoma)
- Facial flushing
- Site infections. Infections cause pain, redness, and swelling.
- Vision changes, such as blurred vision
- Fat loss at the injection site. Fat loss may result in permanent skin dimples.
- Paler skin around the site of the injection
- Temporary increase in blood sugar levels (if you have diabetes)
- Increased blood pressure (if you already have a high BP)
- Headaches (from epidural injections)
- Increased appetite, mood changes, and difficulty sleeping (from blood injections).
When to Call a Doctor?
Seek medical care immediately if you experience the following signs and symptoms:
- Signs of mental health changes. Such changes can include being depressed or anxious and having suicidal thoughts. They may also include mood swings, seeing or hearing things that aren’t there, or having scary thoughts.
- Infection signs (fever, chills, sore throat, ear pain, sinus pain, and a wound that doesn’t heal).
- You have diabetes and notice your usual symptoms changing.
- A "moon face" (a puffy, rounded face) and weight gain in the upper back or belly. These are signs of Cushing’s syndrome.
- Breathlessness, chest pain, and swollen limbs. These can be signs of a deep vein thrombosis (DVT) or a blood clot.
- Vision changes (such as blurred vision)
Takeaway
Steroid injections, such as cortisone shots, are generally safe. They’re used for pain and inflammation relief in different parts of the body.
In some cases, steroid shots may hit a nerve when injected through the skin. As a result, the affected nerve may become injured and damaged.
A steroid injection may hit a nerve for the following reasons:
- The needle is incorrectly placed
- Anatomic variations are not considered
- The doctor lacks experience and concentration
Just because you have nerve damage does not mean a cortisone shot is the cause. Surgical procedures are a common iatrogenic (doctor-inflicted) cause of nerve injuries.
An injection may result in nerve injuries by:
- Directly damaging the nerve
- Causing a hematoma
- Causing an infection
- Cutting off the blood supply to a nerve
- Administering the wrong drug
Common symptoms of nerve damage include the following:
- Neuropathic pain (sharp, shooting, or burning pain)
- Numbness (Loss of sensation)
- Tingling or prickling
- Muscle weakness and wasting
- Changes in the way you feel pain
Feeling transient pain that lasts for a few days after receiving an injection is normal.
More severe symptoms, such as paralysis, may happen if the injection hits a group of nerves.
Permanent nerve damage after a cortisone shot is rare. Recovery from the side effects depends on how severe the nerve injury is.
Most people take a few days to a few weeks to fully recover from mild single-nerve injuries. For more severe damage, recovery may take months or years.
To avoid affecting a nerve when giving a cortisone shot:
- Healthcare providers should have experience and adequate preparation.
- You should cooperate with the doctors during the injection.
- You should stop taking any blood thinners a few days before to prevent bleeding.
- Sterile conditions are necessary to avoid contamination and infection.
- Your condition should be evaluated after receiving the injection.
Doctors recommend you take no more than three or four cortisone injections per year for any body region.