At some point, everyone's had meals so good that they couldn't help but get seconds and thirds. But then, some time afterward, many of us have paid the heavy price of overstuffing ourselves: the lump in the throat won't go away, the annoying cough, and the bitter taste in the back of the mouth. Maybe you've even felt neck pain when having acid reflux. What's the deal? Let's get into the skinny of whether it's reflux causing your neck pain.
Can Silent Reflux (LPR) Make Your Neck Hurt?
According to the American Family Physician Journal, GERD (in which silent reflux could be considered a subtype) can cause neck pain in some patients.
Furthermore, the same journal lists another two neck-pain-inducing mechanisms as additional symptoms:
- Chronic coughing and
- Constant throat clearing.
The repetitive muscle contractions involved in these actions can strain the neck muscles, leading to muscle fatigue, tension, and inflammation.
As a result, individuals may experience aching, soreness, or sharp pain in the neck. Addressing these symptoms promptly is crucial to prevent escalating discomfort and potential complications.
Silent reflux or Laryngopharyngeal Reflux (LPR) is a condition that can make be very uncomfortable on the throat and voicebox. Persons with LPR may feel the urge to cough or clear their throat repeatedly, making it painful. The condition is often related to acid reflux, which is when acid from the stomach goes back up into the esophagus.
Acid Reflux (GERD) and Silent Reflux (LPR)
"Reflux" refers to when stomach acid (typically confined to the stomach) flows back into the esophagus. In a healthy person, the esophagus's lower muscles stop food from returning to the stomach. When these muscles are weak, reflux happens.
Up to this point, GERD and LPR are identical.
Still, some other key differences exist:
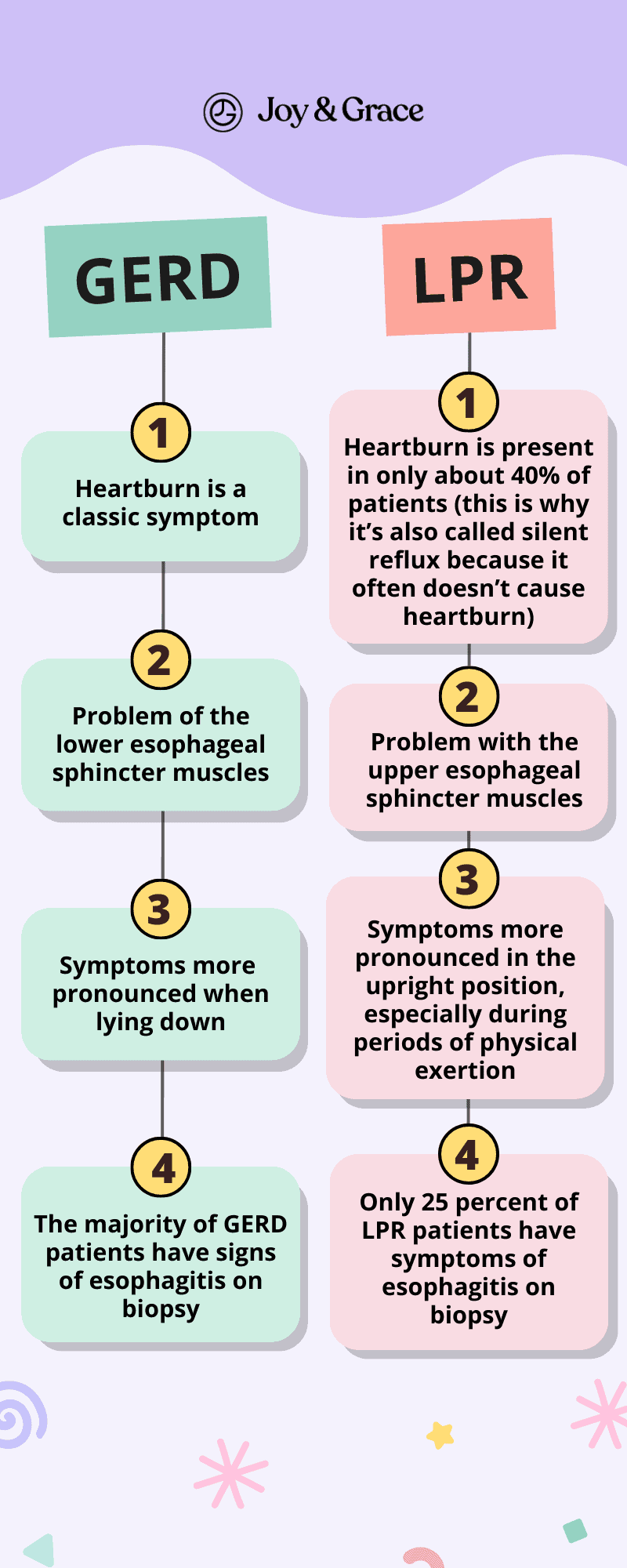
Understanding these differences is important for diagnosing GERD and LPR correctly and treating them in the right way.
There are different ways to treat GERD and LPR.
For GERD, the focus is on reducing acid production and making the lower esophageal sphincter stronger.
For LPR, the focus is on protecting the upper airway and reducing acid exposure. People with acid reflux symptoms can get personalized advice from a medical professional.
Where Do You Feel Silent Reflux (LPR)?
People often think of heartburn or chest pain when they think of “reflux,” but those aren't the usual signs of silent reflux. Instead, the irritation and hoarseness are felt in the back of the throat and affect the voice.
The reflux reaches these parts of the body and irritates them, causing coughing, a lump in the throat feeling, and other symptoms. Sometimes people with silent reflux may also feel pain in the neck and shoulder area.
To sum it up, according to a study with 225 patients, the most common symptoms in people with LPR are:
- Abnormal or hoarse voice - 71 % of patients,
- Cough - 51 % of patients
- Globus (feeling of something in your throat) - 47 % of patients,
- Excessive throat clearing - 42 % of patients
- Dysphagia (swallowing problems) - 35 % of patients
Do Symptoms of Silent Reflux (LPR) Come and Go?
Yes, silent reflux symptoms (LPR) can come and go based on various factors.
Certain behaviors or dietary choices can exacerbate LPR symptoms, causing them to "come" or become more noticeable.
For example:
- Acidic, spicy, or fatty foods,
- Caffeine,
- Alcohol, or
- Carbonated drinks can make the symptoms of acid reflux worse.
On the other hand, people with LPR may see their symptoms "go away" or lessen when they try to change how they act and follow their doctor's advice.
LPR symptoms can be relieved by making changes to your lifestyle, such as:
- Avoiding "trigger foods"
- Practicing portion control,
- Giving up smoking,
- Dealing with stress, etc.
We’ll be discussing these in more detail just a bit later in the article.
Can Silent Reflux (LPR) Cause Swollen Lymph Nodes in The Neck?
Silent reflux (LPR) is not considered a cause of swollen lymph nodes in the neck.
It is important to note that swollen lymph nodes can have various underlying causes, and self-diagnosing or assessing lymph nodes on your own is not advised. If you notice swollen lymph nodes or have concerns, it is recommended to consult with a healthcare provider for proper evaluation and diagnosis.
How Long Does Silent Reflux (LPR) Flare-Up Last?
The duration of a silent reflux flare-up can vary from person to person. For some, an episode may last for only a few days. For others, it may last for weeks or even months. Some of the bothersome symptoms can show up during the day, especially when speaking or doing things that need your voice.
Some people find that specific lifestyle changes can help reduce the frequency and severity of their symptoms. Some small changes that can make a big difference are avoiding trigger foods, eating smaller meals more often, and not lying down right after a meal. Others may need to take medication regularly to keep their symptoms under control.
How Do You Treat Silent Reflux (LPR)?

Laryngopharyngeal reflux (LPR) is first treated by changing the person's diet and behavior.
Doctors typically don’t prescribe any medication until these measures fail. Let’s review what kind of diet and lifestyle modifications you can make to feel better.
Changes To The Diet
Caffeine-containing foods and drinks weaken the protective esophageal sphincters that keep acidic contents in the stomach and esophagus and should be avoided. Those include:
- Coffee,
- Tea,
- Soda, and
- Energy drinks, as well as
- Alcohol,
- Chocolate, and
- Peppermints,
Chocolate and peppermint contain chemicals similar to caffeine. They cause the stomach to make more acid and weaken the upper esophageal sphincter. Even decaffeinated teas and coffees still have caffeine. Choose caffeine-free drinks.
High acidic and spicy foods should also be avoided. Those include:
- Most fruits
- Citrus fruits
- Tomatoes
- Jams and jellies
- Barbecue sauces
- Salad dressings
Even though many of these foods are healthy in other ways, they can worsen reflux at the larynx level. People with severe symptoms should try to find less acidic alternatives.
Don't drink drinks with carbonation. Many have caffeine, which relaxes the sphincters and makes stomach acid come up when you burp. The effects of carbonated drinks with alcohol are the same. Even carbonated drinks without caffeine, like seltzer water, can make you burp. Each burp can cause reflux of stomach acid and enzymes into the laryngopharynx.
Lifestyle Modifications
Using common sense can limit LPR symptoms:
- Nicotine in cigarettes makes your body produce more acid, which is why you should not smoke.
- The more the stomach is swollen, the more likely its contents will spill into the esophagus.
- It's best to eat smaller meals throughout the day rather than big lunches and dinners.
- Vigorous exercise should be avoided for at least two hours after a meal.
Patients should also avoid filling their stomachs too much with fluids during or right before exercise. However, they should still be properly hydrated to exercise. - Patients should not eat or drink for three hours before going to sleep.
Even though LPR doesn't usually happen when a person is lying down, some patients (especially those who eat close to bedtime) may also benefit from raising the head of the bed to let gravity help keep gastric contents from coming back up.
Doctors may prescribe drug therapy if diet and behavior modifications don’t work.
What Is the Best Medicine for Silent Reflux (LPR)?
If lifestyle changes alone can't relieve silent reflux, medications are usually the next step in treatment. Although, their use is a bit controversial.
For example:
In the absence of esophageal GERD syndrome, the American Gastroenterological Association recommends against proton pump inhibitors (PPIs) or H2 blockers.
On the other hand, The American Academy of Otolaryngology-Head and Neck Surgery says that most people with LPR should take PPI twice a day for at least six months.
Nevertheless, as stated above, the first-line medical treatment drugs for LPR are:
- Proton pump inhibitors (PPIs) help stop reflux by reducing stomach acid production. The stomach releases less acid when digesting food by blocking enzymes. This reduces the chances of it spilling into the esophagus and throat. Some of the more common PPIs are omeprazole and lansoprazole.
- Antacids use pH to directly neutralize excess acid in the stomach. Compared to PPIs, antacids are faster at providing relief but are short-lasting. On their own, they can't address the root problem of reflux, where too much acid is being produced.
A doctor can also give you histamine-2 receptor antagonists (H2RAs) such as ranitidine, cimetidine (Tagamet), or famotidine (Pepcid). These also reduce acid in the stomach, using a different mechanism than PPIs. Prokinetics are another type of medicine that makes the stomach work harder to move its contents to the small intestine. This makes reflux less likely. Surgery is rarely an option for some people with LPR. It is usually only considered if other treatments of LPR have not worked.
Which PPI Is Best for LPR? Is Omeprazole Good for Silent Reflux (LPR)?

One of the most commonly prescribed PPIs for silent reflux disease is omeprazole. Omeprazole is considered one of the best drugs in its class for eliminating silent reflux symptoms. As a perk, it has fewer side effects when taken at recommended doses for people with LPR.
Omeprazole is a proton pump inhibitor (PPI) that reduces the amount of acid the stomach produces. This can help to relieve symptoms of LPR, such as heartburn, chest pain, and throat irritation.
In some cases, though, omeprazole may interact with other medications a person might take. Blood thinners like clopidogrel and other drugs like diuretics, digoxin, and antivirals are among them. Before taking any new medicines, it's best to talk to a licensed doctor to get the correct information about whether this medicine is right for you. An alternative may be better suited to your specific needs.
How Long Do PPIs Take to Work for Silent Reflux (LPR)?
PPIs are usually taken once or twice daily, depending on the specific medication. In total, you may need to continue treatment for two to three months or longer. It can take weeks or months of PPI treatment to notice improvement. Usually, slight improvement happens after the first few weeks. More severe cases of LPR may require longer-term PPI treatment. A higher dose may also be needed to achieve symptom relief.
Talk to your healthcare team if you have been taking PPIs and don't feel better. They may recommend adjusting your dose or trying a different type of medication.
Do ENT Doctors Treat LPR?
Otolaryngologists, or Ears, Nose & Throat (ENT) doctors, are specialists in treating this region of the body. Some ENT doctors even focus on treating coughing and voice changes caused by laryngopharyngeal reflux (LPR).
Some ENT doctors treat LPR, but not all do. Talk to your doctor about any symptoms that make swallowing hard or uncomfortable. Before making an appointment, ask your doctor if they treat this condition.
Can LPR Be Cured Permanently?
In the strictest sense, LPR cannot be ultimately "cured." When a person begins to have reflux symptoms, the shape of certain body parts has changed over time, like the sphincter or “door” between the stomach and the esophagus. This can be due to swelling or scarring, but generally, this sphincter will be prone to leaking acid.
Because of this, people with reflux will always be at risk of flare-ups, LPR included. This is especially true when lifestyle factors and triggers for reflux are left unchecked.
The good news is that with some attention and effort to prevent flare-ups, it is possible to live a symptom-free life from silent reflux. For many people, lifestyle changes alone are enough to remove the symptoms of LPR. During nasty flare-ups, pain, and discomfort can sometimes be eased with short-term medication like antacids. When silent reflux is bad, you may need to take medicine for a long time, but you can still control the symptoms and make them less noticeable.
If you have LPR, working with your doctor to determine a treatment plan for you is crucial. You can keep your symptoms under control and live an everyday, healthy life if you know how to treat them.
Takeaway
Silent reflux, or LPR, can be a nagging problem with dry cough and neck pain for people suffering from gastroesophageal reflux disease. The excess acid spilling from the stomach can irritate the throat and voicebox, leading to hoarseness, voice changes, and neck pain. While the problem can last for minutes at a time, there's no need to suffer in silence. With the help of lifestyle changes and guided treatment, silent reflux can be kept in check.
Are you itching to tell us about your experience with silent reflux, or have you been relieved of it? Tell us more below and stay updated with our other articles about health topics.