According to a study published in the Journal of Headache and Pain in 2022, 15.8% of the world's population experiences a headache daily. Women may experience headaches due to hormonal changes or before their period. While these may persist for more than a day, frequent spells of headache may need medical attention.
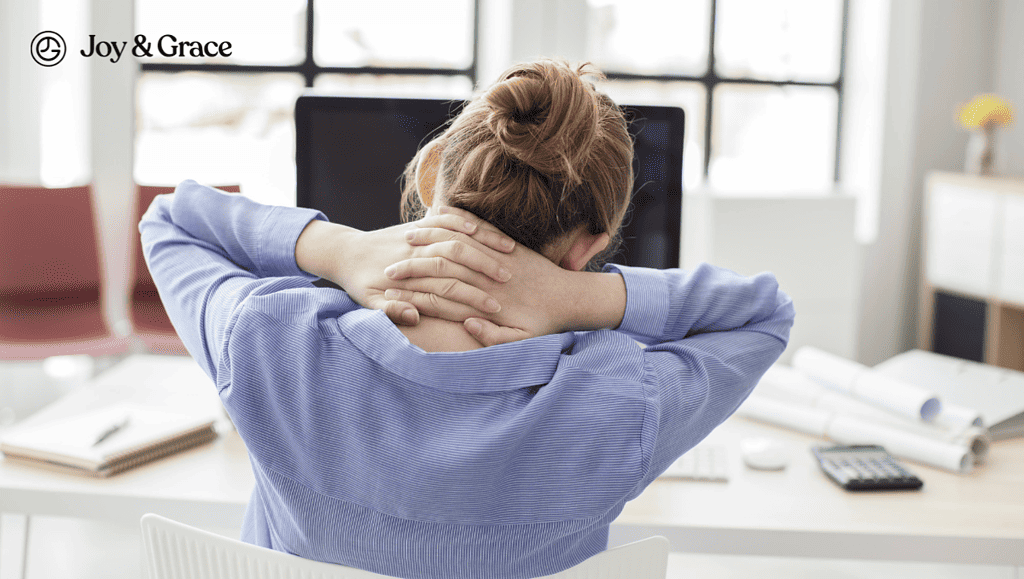
Bad posture, how you sleep, and bacterial or viral infections can also cause neck pain.
Migraine headaches are mostly known to be accompanied by symptoms such as sensitivity to light and sound. But are nausea and neck pain additional migraine symptoms? According to a recent study by the American Migraine Foundation, the answer is yes. In fact, neck pain is a more frequent symptom of migraine than nausea. Did you know neck pain can also indicate an incoming migraine attack?
Let’s start reviewing all these and more.
Why Do My Neck And Head Hurt, And I Feel Nauseous?
The most common cause of headaches accompanied by nausea and neck pain is migraines.
A systematic review conducted in 2022 concluded that 77% of patients experiencing migraine also reported neck pain. It was also found that people with chronic migraines complain about neck pain more often than people with episodic migraines.
Given that neck pain is associated with migraines, you need to know what exactly a migraine headache is.
A migraine headache is a type of headache associated with sensitivity to light and sound, that feels like a throbbing pain on one side of the head.
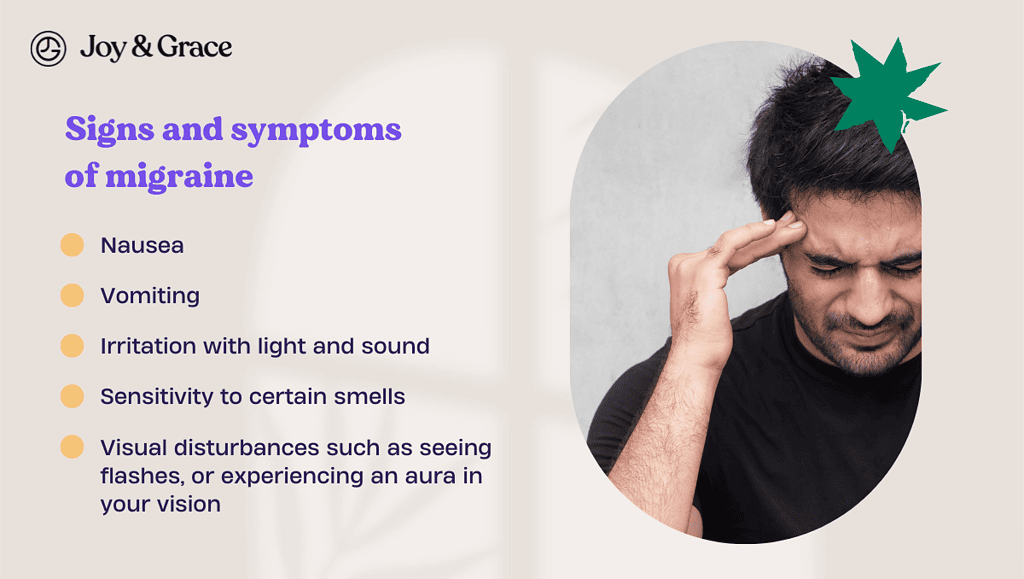
The primary symptom of a migraine is the headache itself. But migraines can also be accompanied by additional symptoms, such as:
- Nausea
- Vomiting
- Irritation with light and sound
- Sensitivity to certain smells
- Visual disturbances such as seeing flashes, or experiencing an aura in your vision.
Hence, if you’re experiencing continuous head and neck pain and are nauseous, it may be an indication of a migraine.
Can A Migraine Make Your Neck Hurt?

Neck pain is a very common side effect of migraines, as we previously mentioned.
However, it is important to understand that neck pain is only a symptom and not a cause of migraine.
Learning about the link between migraines and neck pain is also useful. Here’s how it goes:
A nerve called the “trigeminal nerve” (which is the fifth cranial nerve) is present in the highest point of the cervical spine, which is in the neck. It is formed by a bundle of nerves extending from the brain to the face and has three main branches supplying the muscles of the face and neck.
Extensive research has shown that migraines occur due to the overactivity of neurons in the trigeminal nerve.
During a migraine attack, unusual nerve signals from the trigeminal nerve also trigger its branches in the face and neck. These branches send pain signals and release substances that result in telltale signs of migraine: nausea, vomiting, and neck pain.
Can Neck Problems Cause Migraines?
As we mentioned earlier, neck problems are not known to be the cause of migraines.
However, since we’re talking about headaches, neck problems can definitely cause other types of headaches that are very similar to migraine headaches.
Here’s how neck problems can cause those headaches:
The part of the bony spine in the neck is called the cervical spine. Some nerve roots emerge from the spinal cord just below our brain, passing through the gaps between the cervical spine. If any nerve root is compressed, it can cause a headache which may have symptoms like a migraine. This kind of headache is called a cervicogenic headache.
Cervicogenic headaches can be caused by injuries to the neck, such as those encountered in a road traffic accident. They can also be caused by arthritis of the cervical bones, tumors, or even if you have slept in an incorrect position.
A cervicogenic headache is a headache that usually occurs on one side of the head. It is a headache that starts in the neck, gets worse when you move your neck, and might also make you feel nauseous.
If you want to read more, we have a section about cervicogenic headaches here.
Can Cervical Stenosis Cause Migraines?
Cervical stenosis is a condition where the spaces between the cervical vertebrae are narrowed. This compresses the nerve roots that exit the spinal cord to supply different parts of the body. Nerve roots may be pinched, resulting in irritation and subsequent symptoms in the part of the body they supply.
Cervical stenosis may occur due to many causes, two of the most common of which are:
- Bone overgrowth - due to osteoarthritis.
- Bulging disk - Aging causes the intervertebral discs to flatten, bulging into the spinal nerves near the disc.
Symptoms of cervical stenosis are similar to those of cervicogenic headaches, which include headaches accompanied by neck pain. But cervical stenosis can also make the arms or legs on the same side feel numb or tingly, depending on where the nerve is being pinched.
How Do I Know If My Headache Is A Brain Tumor?
Conventionally, doctors thought persistent headaches might be a sign of a brain tumor. Recent studies, however, have shown that tension or migraine headaches are more likely to cause headaches that don't go away than brain tumors.
According to Hopkins Medicine, this is because the brain doesn’t generate any pain signals on itself. If a tumor grows in the brain, it must press on a blood vessel or nerve inside the skull to send pain signals and cause a headache.
To get to the point, it is very useful to know about other symptoms associated with a brain tumor, which can be alarming if they occur with a headache. These include:
- Weakness and numbness on one side of the body.
- Difficulty in speaking
- Difficulty in maintaining posture and balance.
If you want to read more, the International Classification of Headache Disorders ICHD-3 is an extensive guideline for diagnosing primary and secondary headaches.
Based on the guidelines, to put it simply, a headache associated with a brain tumor may be worse in the morning, and it may also be accompanied by nausea or vomiting. However, radiological investigations like an MRI or a CT Scan should show a definite lesion in the brain for a brain tumor to be considered.
Only the definite presence of a tumor in the brain can label the headache as a headache due to a brain tumor.
If not, the doctor must use other lab tests to determine what's causing the headache and compare that to the ICHD-3 guideline.
How Long Does a Headache From Covid Last?
Studies suggest that the average headache time starts within 24 hours of COVID infection and lasts about seven days.
This is according to a study published in 2021 titled Frequency and phenotype of headaches in COVID-19. In the study, in which 2194 adults participated, headache was reported to be the most common symptom of COVID-19.
According to another article in the Journal of Headache and Pain, headaches are one of the most common side effects after COVID-19. This type of headache is part of the Long COVID syndrome.
Long COVID syndrome headaches can feel like tension headaches and make you sensitive to light and sound, just like a migraine. As was said above, headaches may occur more often during or after COVID, but after about a month, they get less bad and also happen less often.
If you want more detail: Headache in COVID was found to occur more in the forehead. Long COVID headaches were more common in middle-aged women, especially those with chronic headaches.
What Should I Do if I've Had a Headache for 3 Days?
Only people suffering from migraine headaches understand how debilitating they can be.
If a migraine headache doesn't go away after two or three days, you may consider getting support from your workplace and friends. Taking a day or two off work to rest and relax is also recommended. Also, it might be better to ask a family member or friend for help with cleaning and cooking than to buy over-the-counter pain medication.
Long-lasting headaches can also be treated by sleeping enough and avoiding caffeine and alcohol. You can also list your daily activities and routine to identify possible headache triggers, such as excessive screen time or sun exposure (a headache diary).
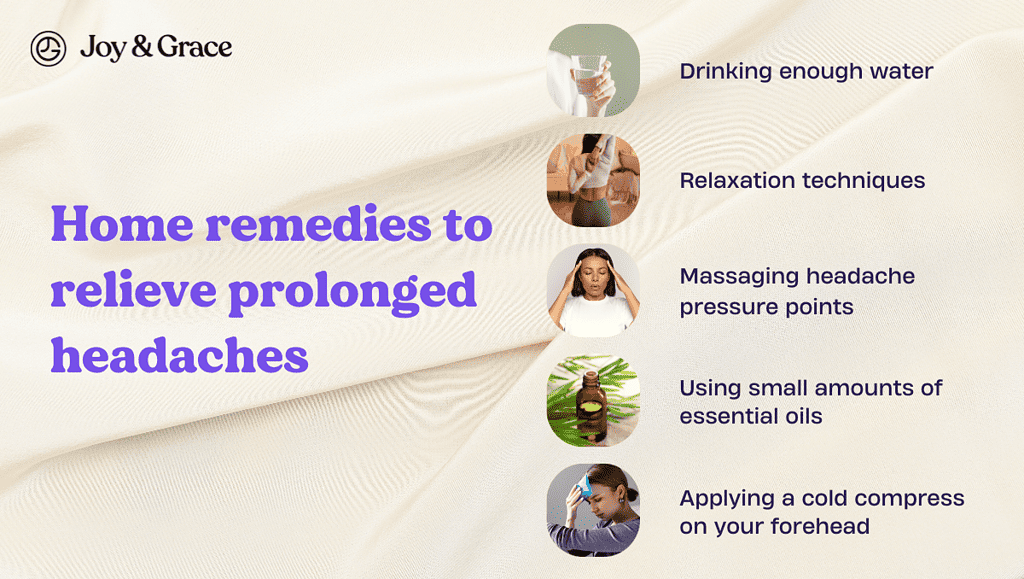
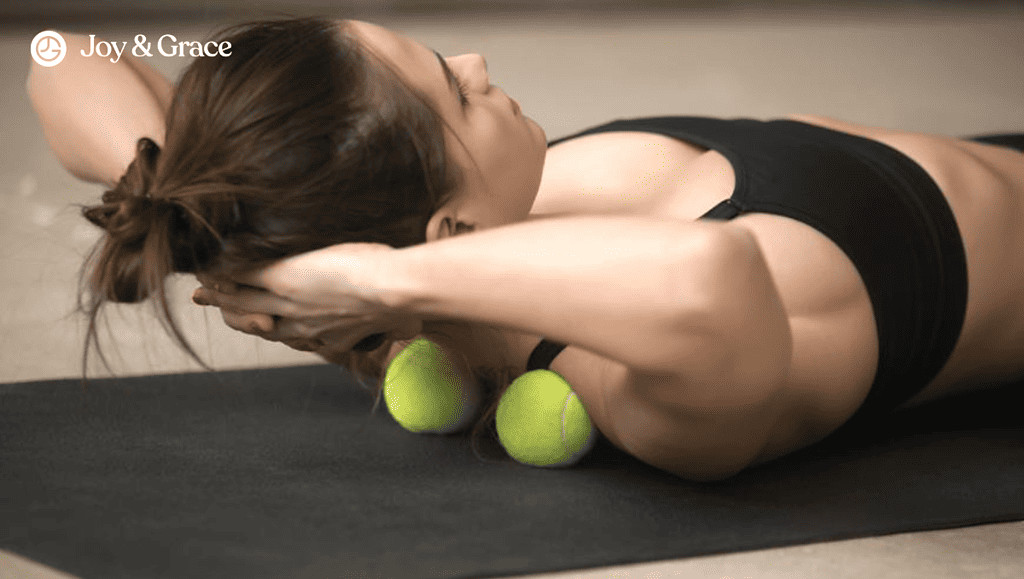
Other home remedies that may relieve prolonged headaches include:
- Drinking enough water.
- Relaxation techniques such as deep breathing exercises or playing relaxing music.
- Massaging headache pressure points, such as rubbing your temples in a circular motion.
- Using small amounts of essential oils, such as lavender or peppermint oil, on your temples.
- Applying a cold compress on your forehead to soothe the headache.
It might be important to know that some headaches, like tension-type headaches (TTH), can be caused by factors such as stress at work, anxiety, or lack of sleep. In this case, it would be better to figure out what's causing the headache instead of just taking over-the-counter painkiller drugs.
When Should You Visit the Hospital for a Headache?
If you're experiencing frequent, worsening headaches, consult your physician. Persistent headaches can indicate any underlying health problem, like a viral infection or a tumor.
New-onset and severe (“worst headache of my life”) headaches also merit prompt medical care.
We would recommend visiting the emergency department of the nearest hospital if you are experiencing any of the following symptoms:
- A sudden, severe headache
- Difficulty in understanding speech
- Inability to speak or see (double vision or complete loss of vision)
- Trouble maintaining balance while walking.
- Stiff neck
- High-grade fever of more than 102 F (or 39 C)
Takeaway
Diagnosing a definite cause of persistent headaches is still a challenge. Even though modern medicine has come a long way, there still needs to be a surefire headache-eliminating therapy. Keeping a healthy weight, living an active life, and knowing when to rest and relax are all essential ways to avoid headaches. Avoidance is the best type of migraine treatment, after all.