Every year in the United States, 1.3 million lucky ladies get to join the menopause club. It usually starts when they're around 51-52 years old. But for some daring dames, they get to start the party early, with early menopause hitting about 5% of women aged 40-45.
If you're a woman experiencing menopause or perimenopause, you might be all too familiar with hot flashes, night sweats, and mood swings. But did you know that shoulder pain can also be a common symptom of hormonal changes during this time?
Make sure you’re comfortable as we'll explore the link between menopause, perimenopause, and shoulder pain. We'll also provide some natural remedies and supplements that can help alleviate the discomfort.
Does Menopause Make Your Shoulders Hurt?

Shoulder pain is a common problem that can be caused by many factors, and menopause is thought to be one of the possible causes. During menopause, a woman's body undergoes many hormonal changes. And these changes can affect the musculoskeletal system as well. All that can lead to various aches and pains, with shoulder pain being no exception.
One possible reason for shoulder pain during menopause is reduced estrogen production. Aside from being the primary female sex hormone, estrogen is a hormone that also helps maintain bone density and strength. As estrogen levels decrease, bones can become weaker and more prone to fractures, including those in the shoulder area.
Another possible cause of shoulder pain during menopause is the development of arthritis. Menopause can increase the risk of developing arthritis, a joint disease that can cause:
- Pain
- Stiffness
- Swelling in the shoulders and other joints.
Rotator cuff tears, a type of shoulder injury, also appear to be more common among menopausal women. In one study, full-thickness tears were more common in postmenopausal women and occurred in about 8.9% of these women.
If you’ve browsed the web, you might’ve noticed some articles mentioning frozen shoulder disease as another possible cause of shoulder pain during menopause. But is that really the case?
Can Menopause Cause Frozen Shoulder?
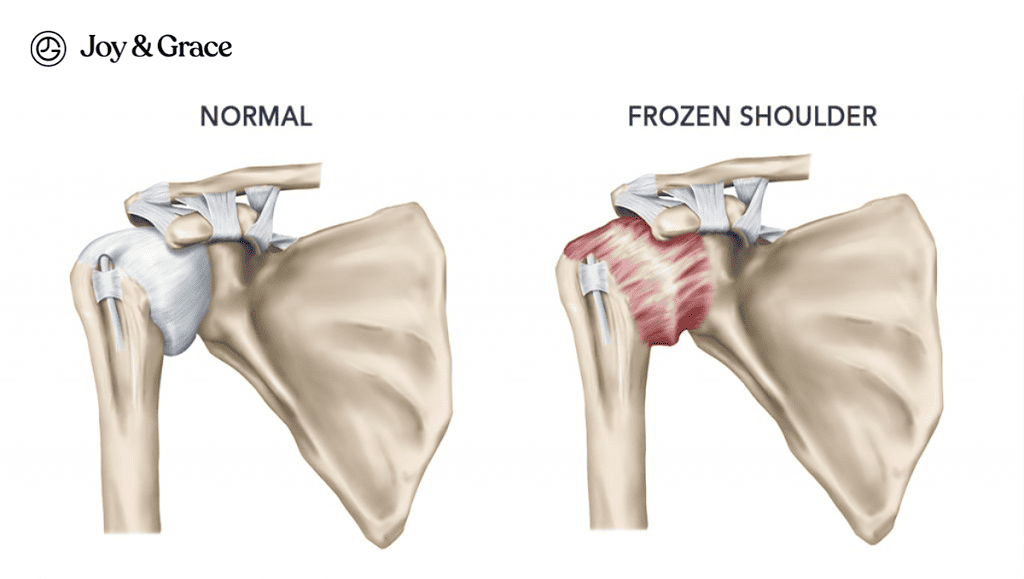
Some studies report a correlation between menopause and a frozen shoulder. However, the exact nature of the relationship needs to be better understood.
Frozen shoulder, also known as adhesive capsulitis, is when the shoulder joint becomes stiff. It can, unfortunately, cause severe pain as well.
This medical condition can make it very difficult for you to move your shoulders. The exact cause of frozen shoulder is still unknown. However, it is more common in women than men and is more likely to occur in people over 40.
There is a chance that the changes in hormone levels that happen during menopause could be the culprit of frozen shoulder in women. In a 2020 study, women with frozen shoulder were more likely to be postmenopausal and have low estrogen levels than women without the condition.
According to Dr. Anne Ford, associate professor in the Department of Obstetrics & Gynecology at Duke University School of Medicine, “Given that older women are most commonly affected by adhesive capsulitis, there may be a connection between the loss of estrogen in menopause and this painful shoulder condition."
Does Perimenopause Cause Shoulder Pain?
Perimenopause is the transitional period before menopause. This period is when a woman's hormone levels begin to fluctuate. This can cause various symptoms, including:
- Hot flashes
- Psychological issues
- Musculoskeletal problems like joint pain.
One study found musculoskeletal symptoms to be especially common in East Asian women during perimenopause. And guess what? Shoulder pain was the most common of all the symptoms.
In the same study, shoulder pain was also common among their perimenopausal participants. 35.4% were diagnosed with adhesive capsulitis or frozen shoulder, and 25.1% had shoulder synovitis.
The cause of these symptoms is not fully understood, but estrogen appears to protect against joint pain and stiffness. As estrogen levels decrease during perimenopause, women may experience more musculoskeletal problems.
Does Menopause Cause Neck Pain?
As if hot flashes and mood swings (and apparently shoulder pain) weren't enough, menopause can also bring on the joys of neck pain. We discuss more in-depth about the relationship between menopause and neck pain here.
Can Menopause Cause Whole Body Pain?
When women reach menopause, more than half of them report experiencing musculoskeletal pain. This also includes joint pain. Joint pain tends to be highest among women aged 45 to 55 years old.
This could be related to menopause and the decrease in estrogen levels.
But it's challenging to prove because musculoskeletal pain is common throughout a person's life. However, women are about twice as likely to experience joint pain and stiffness around the time of menopause compared to when they were premenopausal and of the same age.
What Helps With Menopause Aches And Pains?
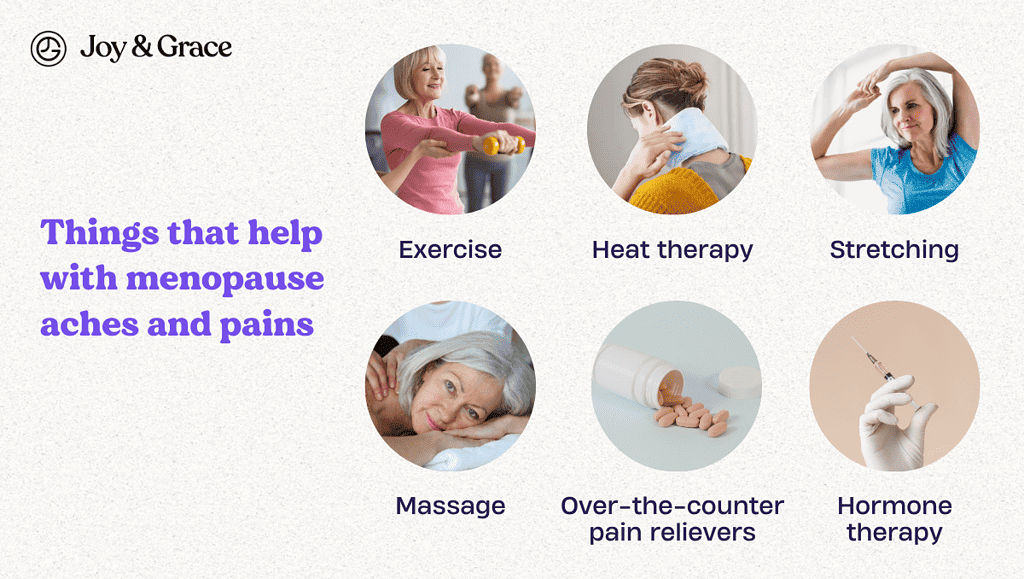
Ladies, don't let menopause throw you off your game! If you're feeling shoulder pain and stiffness, there are some easy steps you can take to get back to your fabulous, shoulder-shimmying self. Here are some tips to help you out:
- Exercise
Regular exercise can help improve joint and muscle strength. Exercise can also reduce stiffness and increase flexibility and range of motion. Low-impact activities such as swimming, cycling, and yoga can be particularly helpful.
- Heat therapy
Applying heat to sore or stiff joints can help alleviate pain. A warm bath, hot water bottle, or heating pad can be effective. If you want a heating pad with an array of relaxing aromas, we have the perfect one for you.
- Stretching
Stretching exercises can help improve flexibility, reduce stiffness, and alleviate muscle tension. Gentle stretches before bed may also improve sleep quality.
- Massage
Massage therapy can help improve circulation, reduce muscle tension, and alleviate pain. It may also improve sleep quality.
- Over-the-counter pain relievers
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help alleviate pain and inflammation.
- Hormone therapy
Hormone replacement therapy (HRT) can also help alleviate menopausal joint and muscle pain. Hormone therapy works by replacing the estrogen the body no longer produces.
Does Joint Pain From Menopause Go Away?

Joint pain is one of the symptoms of menopause and can be frustrating and uncomfortable. The good news is that, in most cases, joint pain related to menopause is not permanent and can go away on its own or with treatment.
In some women, joint pain may go away on its own as their bodies adjust to the hormonal changes that occur during menopause. For others, lifestyle changes may help alleviate joint pain.
What Helps With Menopause Joint Pain?
Aside from those we mentioned earlier, these two can also help relieve joint pain brought about by menopause:
- Diet
Eating a healthy and balanced diet can help reduce inflammation in the body. Incorporate plenty of fruits, vegetables, whole grains, and lean protein into your diet.
- Supplements
Certain supplements can help reduce joint pain and improve joint mobility. It's important to talk to your doctor before starting any new supplements.
What Supplements Help Menopause Joint Pain?
Here are some supplements that have been shown to be potentially helpful for menopause joint pain:
- Glucosamine
Glucosamine is a natural compound found in cartilage and is often used as a supplement to help improve joint health. Some studies suggest that glucosamine may help reduce joint pain and stiffness.
- Chondroitin
Chondroitin is another natural compound found in cartilage. Chondroitin is often combined with glucosamine as a supplement for joint health. It may help reduce inflammation and improve joint mobility.
- Omega-3 fatty acids
Omega-3 fatty acids are healthy fats found in fish oil and other sources. They have anti-inflammatory properties and may help reduce joint pain.
- Soy products
Soy isoflavones are plant compounds similar in structure to estrogen. Since they may mimic estrogen, these compounds may help alleviate menopause symptoms. Some studies suggest that soy isoflavones may help relieve joint pain by reducing the joint degradation that may occur with decreased estrogen levels.
- Vitamin D
Vitamin D is essential for strong bones and may help improve joint health. Getting enough vitamin D is essential, as deficiency can weaken bones and increase joint pain. You can get an adequate amount of vitamin D through a combination of the following:
- Sun exposure
- Diet
- Supplements
- Calcium
Calcium is important for bone health and may help reduce joint pain in women experiencing menopause-related bone loss.
- Magnesium
Magnesium is an essential mineral that plays a role in muscle and bone health. It may help reduce inflammation and improve joint mobility.
Takeaway
If you're a woman going through menopause, you might be experiencing a wide range of musculoskeletal problems. This can range from shoulder and neck pain to joint pain.
This may be because menopause can cause a reduction in estrogen levels. A drop in this vital sex hormone can lead to bone density loss and may increase the risk of developing arthritis.
Additionally, some studies report an association between menopause and painful shoulder conditions, like rotator cuff tears and frozen shoulder.
Fortunately, there are ways to alleviate menopausal aches and pains, even in the comfort of your own home. While joint pain related to menopause is not permanent, taking care of your body is essential to help alleviate the pain.
Stay up-to-date with our latest articles and tips by subscribing to our newsletter. Don't miss out on valuable insights that can help you feel your best during this important time of life. Subscribe today!