Are you tired of dealing with neck pain that just won't go away? You're not alone! Hormonal imbalances can be a sneaky culprit behind these types of symptoms. But don't worry. We're here to shed some light on the subject and give you some tips on alleviating the pain.
In this blog post, we'll be talking about the hormones that can cause neck pain and headaches and the treatment options available. So grab a cup of tea, and let's dive in!
Can Hormone Levels Cause Neck Pain?
For many years, our hormones, especially estrogen, have been linked to numerous pain disorders. These include migraines and jaw disorders. It turns out that estrogen actually increases our sensitivity to nerve injury and mechanical pain. At the same time, other hormones can cause muscle tension or pain.
So how does this relate to neck pain? Well, neck pain can either be neuropathic or mechanical in nature. While hormones don’t necessarily cause neck pain, they may increase your sensitivity to pain. This is especially true during periods of hormonal fluctuations, like during menstruation.
What Are The Hormones Associated With Neck Pain?
The hormones that are usually associated with neck pain are the following:
- Thyroid hormones - Thyroid hormones are produced by the thyroid gland. They play a crucial role in regulating metabolism, growth, and development.
- Estrogen - Estrogen is the main hormone in women and is responsible for regulating the menstrual cycle.
- Progesterone - Progesterone is a hormone produced by the ovaries and adrenal glands in women and by the testicles in men. It is crucial in regulating the menstrual cycle and preparing the uterus for pregnancy.
- Testosterone - Testosterone is a male sex hormone responsible for developing the male reproductive organs. It also encourages secondary sexual traits like increased muscle and bone mass and body hair growth.
- Insulin - Insulin is a hormone produced by the pancreas that regulates glucose (sugar) levels in the blood. It allows the body to use glucose for energy and helps store excess glucose in the liver and muscle tissue.
- Cortisol - Cortisol is a hormone that is produced by the adrenal glands in response to stress. This hormone is responsible for your “fight or flight” response.
How Do Hormones Cause Head And Neck Pain?
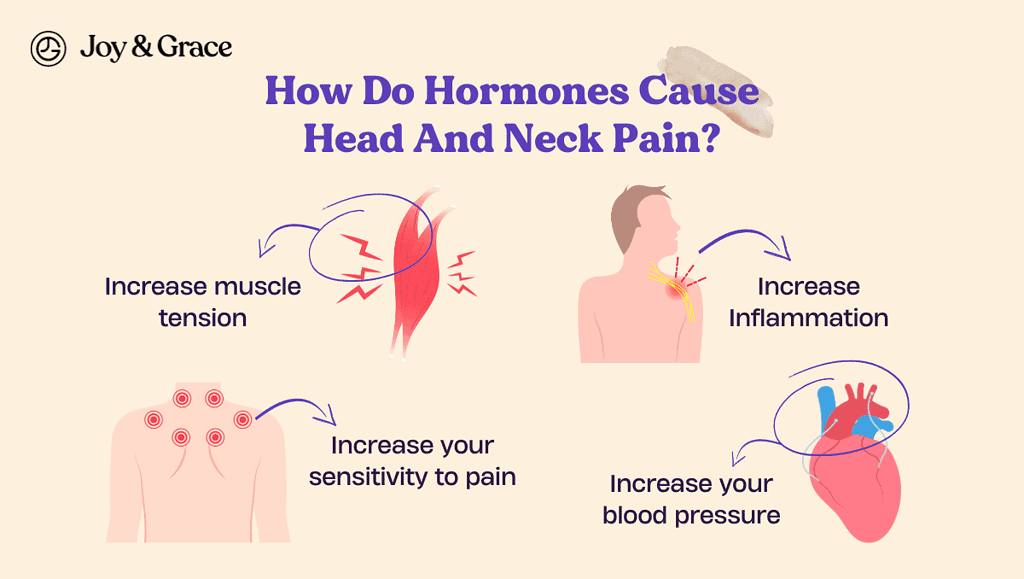
Hormones actually play an important role when it comes to pain. Some hormones have an analgesic effect, which means they decrease pain. In contrast, some may have the opposite effect.
Depending on the hormone, they can either:
- Increase muscle tension
- Increase Inflammation
- Increase your sensitivity to pain
- Increase your blood pressure
Can Estrogen Cause Headaches And Neck Pain?
Changes in estrogen levels during the menstrual cycle can cause headaches and neck pain in some women. Additionally, changes in estrogen levels can also lead to migraines in some women.
Estrogen plays a role in regulating the blood vessels in the head, as well as the release of other chemicals that are responsible for pain. The decrease in estrogen levels may increase your sensitivity to pain, leading to menstrual-related headaches.
These headaches typically feel like a steady, aching pain on both sides of the head. They can be accompanied by muscle tension in the neck and shoulders.
Aside from the hormone itself, women actually have a unique estrogen receptor in a specialized cell called a “mast cell.” Mast cells are a type of blood cell of your immune system that releases special proteins called cytokines when they’re activated. These cytokines result in inflammation and may cause muscle pain and cramping.
When estrogen binds to your mast cell, it may release a larger amount of cytokines. This may be why women are more prone to chronic pain and inflammation. According to one study, chronic neck pain, back pain, and migraines were more common in women.
Can Progesterone Cause Headaches And Neck Pain?
There are conflicting studies on whether progesterone can cause pain. In one study done in 2019, progesterone may decrease your pain threshold and increase your sensitivity to pain. However, this study only looked into pain caused by pin-pricks and incisions and may not translate to neck pain.
But many studies agree that progesterone can actually protect you from neuropathic pain or pain from damaged nerves. If your progesterone levels go down, you may be more likely to get neuropathic pain, which can happen anywhere, including in the neck.
And similar to estrogen, progesterone is also linked to headache disorders and migraines.
Can Testosterone Cause Headaches And Neck Pain?
Testosterone is not typically considered a direct cause of neck pain and headaches. However, low testosterone levels can contribute to chronic pain. In a 2017 study, the participants with low testosterone levels had higher pain ratings. According to the same study, low testosterone may directly affect the brain's pain centers in men.
Testosterone has also been linked to diabetic neuropathic pain, a common cause of pain in diabetic patients.
Can Insulin Cause Headaches And Neck Pain?
Insulin probably doesn't cause headaches or neck pain. But changes in insulin levels, especially when they go up and down or get too low, can cause symptoms like headaches and neck pain.
Hypoglycemia can cause headaches, weakness, and tiredness. This can happen as a side effect of diabetes treatment with insulin.
In the same way, having high blood sugar (hyperglycemia) can cause headaches and tiredness. This can happen when insulin therapy is not well-managed.
Low insulin levels may also result in diabetic neuropathic pain. As the sugar levels in your blood continue to increase, they may eventually deposit into your nerves and damage them. Insulin resistance is also linked to osteoarthritis, which may cause neck pain.
Can Thyroid Hormones Cause Headaches And Neck Pain?
Thyroid disorders can also cause head and neck pain as a symptom. Neck pains are pretty common if you have thyroiditis or inflammation of your thyroid gland. Usually, the pain is mainly around your thyroid gland, but it can also radiate to your jaw or ear. However, this is generally due to inflammation and not the direct action of your thyroid hormones.
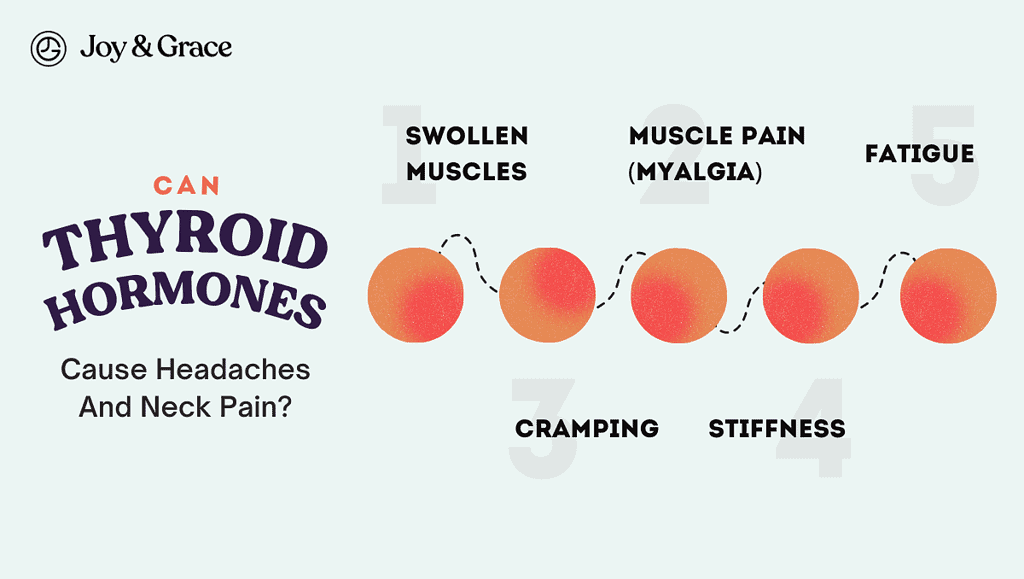
If you have decreased thyroid hormone levels (hypothyroidism), you may experience “hypothyroid myopathy.” This can present as:
- Swollen muscles
- Muscle pain (myalgia)
- Cramping
- Stiffness
- Fatigue
Hypothyroidism is also associated with neuropathy. Neuropathy means that your nerves are damaged and can present as:
- Pain
- Burning or tingling sensation
- Loss of sensation
- Muscle weakness
Hypothyroidism may also make you prone to having more frequent and severe headaches and migraines. In a 2021 study, people with migraines were more likely to have lower thyroid hormone levels than people with other kinds of headaches.
Furthermore, in a study done in 2013, hypothyroidism occurred after the start of migraine episodes in 96% of the participants.
In another study done in 2016, people with migraines had a 41% increased risk of developing hypothyroidism. In comparison, those with other types of headache disorders had a 21% increased risk.
In one case, a headache was the only symptom in a patient with thyroiditis.
Despite all these studies, the connection between thyroid and headache disorders remains unclear.
The IHS came up with criteria to diagnose headaches caused by hypothyroidism. You may be considered to have a headache caused by hypothyroidism if:
| Headache attributed to hypothyroidism - Diagnostic Criteria |
| Have been diagnosed with hypothyroidism |
| Experience head pain on both sides that goes away after hypothyroidism is treated |
| Can show that your hypothyroidism likely caused your headaches, which needs to meet two of these requirements:The headache started before or led to the discovery of the hypothyroidismThe headache got worse at the same time as the hypothyroidism and got better when the hypothyroidism improvedThe headache is:On both sides of the headConstantAnother condition can’t better explain the headache |
Can Cortisol Cause Headaches And Neck Pain?
Stress is one of the most common causes of neck pain and headaches. Cortisol is a hormone that is produced by the adrenal glands in response to stress. High levels of cortisol can cause muscle tension and pain in the neck and shoulders. This is because cortisol can cause the muscles to contract, leading to tension and discomfort.
Cortisol also affects the immune system and modifies the body's response to pain. It affects the brain's reward centers, which can decrease the threshold for pain perception. Basically, cortisol makes you more sensitive to pain.
Chronic stress can lead to persistently elevated cortisol levels. This can exacerbate the problem and make the pain more recurrent, leading to a vicious cycle. Additionally, cortisol can cause inflammation in the body, which can also contribute to pain in the neck and shoulders.
Stress is a big contributor to a number of diseases, and neck pain is on the list. Stress, along with anxiety and depression, are major risk factors for neck pain.
Can Menopause Cause Neck and Head Pain?
While menopause may seem like you're finally free from the troubles of menstruation, it actually comes with its own set of symptoms. During menopause, the body's production of estrogen decreases. And as we mentioned earlier, this can lead to a number of symptoms, including headaches and neck pain.
Additionally, menopause can also increase a woman's susceptibility to migraines. A severe, throbbing pain on the side of the head characterizes migraine headaches. They can be accompanied by other symptoms such as nausea, vomiting, and sensitivity to light and sound.
In menopausal women, the pain is not just limited to the head and neck and may be felt all over the body. In one study, 52% of women with menopause had chronic pain.
What Are Other Symptoms Of Menopause?
In addition to neck and head pain, menopause can cause several other symptoms. Some of the most common symptoms of menopause include:
- Hot flashes
You may experience a sudden feeling of warmth or heat that can cause sweating, flushing of the skin, and a rapid heartbeat.
- Night sweats
These can be due to hot flashes that occur at night, which can disrupt sleep and cause fatigue during the day. This may be because decreased estrogen levels can affect the hypothalamus. The hypothalamus is responsible for regulating our temperature.
- Irregular periods
As you transition towards menopause, it's normal for you to have irregular or missed periods. This marks the end of the menstrual cycle and reflects declining reproductive hormone levels.
- Breast Soreness and changes in breast size
Breast soreness is a common symptom during menopause. This means that the breasts may feel tender or sensitive to the touch. This may also present as a burning sensation.
Although this symptom is common during menopause, it often becomes less frequent during the later stages.
The hormonal fluctuations can also cause your breasts to change in size and shape.
- Decreased Libido
Menopause can also affect your sex drive. Menopause can also affect your sex drive. This can happen because lower hormone levels make it harder for you to feel physically aroused.
Additionally, the other symptoms of menopause, such as mood changes or side effects of medication, can also play a role in lowering libido.
- Vaginal dryness
A decrease in vaginal lubrication can cause discomfort during sexual activity. It can also increase the risk of vaginal infections. This happens because the drop in sex hormones causes a decrease in blood circulation in the vagina.
- Mood changes
These include Irritability, depression, anxiety, or other mood changes. Depression is a common condition triggered by the hormonal fluctuations associated with menopause. Women may feel sad, hopeless, or lack energy, which can lead to difficulty with daily activities.
Anxiety and panic disorder can also develop during menopause. These conditions can cause feelings of fear, worry, or nervousness. Physical symptoms such as increased heart rate, sweating, and shaking can also be experienced.
In one study, 36.8% of menopausal women had depression, while 53.7% had anxiety.
- Sleep Changes
During menopause, a woman's sleep can be disrupted for various reasons. This includes night sweats, waking up frequently, or difficulty falling asleep. This can lead to lighter and more disturbed sleep patterns.
Hormonal changes, stress, and other factors can also contribute to sleep disturbances during this stage of life.
- Fatigue
You may experience extreme tiredness and lack of energy. This may be because of hormonal fluctuation or lack of sleep.
- Weight Gain
During menopause, women often gain weight due to a combination of factors such as hormonal changes, slowing metabolism, and a sedentary lifestyle.
Hormonal changes can lead to an increase in body fat, particularly around the waist. A slowing metabolism means the body burns fewer calories at rest, which can also contribute to weight gain.
Additionally, a decrease in physical activity levels can lead to a buildup of fat and weight gain.
- Bloating and other digestive symptoms
Menopause can cause bloating and other digestive issues due to changes in hormone levels and metabolism. Hormonal changes can slow digestion and cause constipation, bloating, and other digestive discomfort.
Menopause can also alter the intestinal microbiome, the community of microorganisms in the gut. The changes in hormone levels during menopause can impact the composition and balance of the gut microbiome.
A disrupted gut microbiome can also affect how food is digested and absorbed. Furthermore, a change in the gut microbiome can result in increased inflammation and a decreased immune response, which can further contribute to digestive issues during menopause.
- Tingling and Electric Shock Sensations
During perimenopause and menopause, women may experience tingling or electric-shock-like sensations. The exact cause is unknown, but it is believed to be related to hormonal fluctuations impacting the central nervous system.
- Burning Mouth and changes in taste
Burning mouth syndrome (BMS) is a condition that causes a burning or scalding sensation in your mouth, accompanied by changes in taste.
The exact cause of BMS during menopause is unknown, but it is believed to be related to hormonal changes and changes in the nervous system.
The decline in estrogen levels during menopause can affect glands in the mouth responsible for producing mucus. These glands have receptors for sex hormones; as estrogen decreases, the receptors are also affected.
This decrease in hormones can result in pain and discomfort in the mouth. It can also make you more prone to gum disease and cavities. The lack of saliva can create an environment where bacteria can thrive.
- Cognitive changes
These include memory loss, trouble concentrating, or difficulty thinking clearly (brain fog).
- Cardiovascular changes
These include an increased risk of heart disease, stroke, irregular heartbeats, or high blood pressure.
- Skin and hair changes
These can be wrinkles, dryness, brittle nails, and skin and hair thinning. Decreased estrogen levels can affect the skin's ability to retain moisture. This can result in dry, itchy skin.
Estrogen also helps maintain hair growth and thickness, so a decrease in this hormone can make hair thinner and fall out more easily.
Menopause can make your nails weak and easily breakable because your body may not produce enough keratin. Keratin helps keep nails strong. This lack of keratin can lead to brittle, weak nails that crack or break easily.
- Body odor
Menopause can lead to an increase in body odor due to hot flashes and night sweats. Stress and anxiety can also cause a person to sweat more and contribute to body odor.
- Allergies
During menopause, some women may experience new or worsening allergies due to increased histamine. Histamine is the chemical that triggers allergic reactions, and it can spike during menopause.
- Muscle and joint pain
A decrease in estrogen may cause inflammation and decrease the amount of fluid that lubricates the joints. This makes menopausal women more prone to osteoarthritis.
- Osteoporosis
Osteoporosis is a condition where bones become weak and fragile and can break easily. During perimenopause, decreased estrogen levels can lead to a loss of bone density, which in some cases can result in osteoporosis.
- Urinary symptoms
You may have bladder control problems, urinary tract infections, and difficulty urinating.
Menopause can cause problems with bladder control, resulting in the involuntary loss of urine. This can happen because hormonal changes during menopause can affect the muscles in the pelvic area.
Stress incontinence happens when the muscles in the pelvic area are weak. This can lead to leaking urine when you cough, laugh, sneeze, or lift something heavy.
Urge incontinence is when your bladder muscles are too active or easily irritated. This can cause you to suddenly feel the need to go to the bathroom a lot, and sometimes you might leak urine.
In one study, 76% of menopausal women had stress urinary incontinence, while 72% had urge urinary incontinence.
It's important to note that every woman's experience of menopause is unique. Some women may experience more or fewer symptoms than others.
How Do I Know If I Have A Hormone Imbalance?
It can be difficult to know if you have a hormone imbalance without a proper medical evaluation. The symptoms of hormone imbalances can be similar to those of other health conditions and can be caused by various factors.
Hormonal imbalances can cause a wide range of symptoms, some common to both males and females, while others are specific to one gender or the other. Here is a list of signs and symptoms of hormonal imbalance:
Common symptoms:
- Weight gain or loss
- Fatigue
- Muscle weakness, aches, tenderness, or stiffness
- Joint pain, stiffness, or swelling
- Numbness or tingling sensation
- Change in heart rate
- Sweating
- Increased sensitivity to cold or heat
- Constipation or frequent bowel movements
- Frequent urination
- Increased thirst or hunger
- Decreased sex drive
- Depression, nervousness, anxiety, or irritability
- Blurred vision
- Infertility
- Thinning or fine, brittle hair
- Dry skin
- Puffy face
- Stretch marks
- Skin tags
- Acne
- A hump on the neck
Signs and symptoms seen in those born female:
- Heavy or irregular periods
- Hirsutism (excessive growth of facial, chest, or back hair)
- Chronic acne
- Hair loss
- Darkening of skin
- Vaginal dryness or atrophy
- Pain during sex
- Night sweats
- Headaches
Signs and symptoms seen in those born male:
- Gynecomastia
- Breast tenderness
- Erectile dysfunction
- Decreased beard and body hair growth
- Loss of muscle mass or bone mass
- Difficulty concentrating
- Hot flashes
If you are experiencing any of these symptoms, it's best to consult a healthcare provider. Your healthcare provider may order some blood tests to check your hormone levels. They may also refer you to an endocrinologist (hormone specialist) for further evaluation.
Once your doctor has determined the cause, they may suggest the best treatment for your case.
How Do I Fix Hormonal Imbalances?
Fixing hormonal imbalances depends on the specific cause of the imbalance and the individual case. Here are some general treatment options that your doctor may suggest:
Hormone replacement therapy
- Hormonal replacement therapy (HRT) is a treatment used to replace hormones that are no longer produced by the body. HRT is commonly used to treat symptoms of menopause, andropause (male menopause), and hormonal imbalances.
Here's a list of hormonal replacement therapies:
- Estrogen replacement therapy (ERT)
ERT replaces the estrogen that's no longer produced by the ovaries during menopause. It relieves symptoms such as hot flashes, night sweats, vaginal dryness, and mood swings. - Testosterone replacement therapy (TRT)
TRT is used to replace the testosterone that's no longer being produced by the testes in men. TRT can help to improve energy levels, sex drive, muscle mass, and bone density. - Thyroid hormone replacement therapy (THRT)
THRT is used to replace the thyroid hormone that's no longer being produced by the thyroid gland. THRT can help to alleviate symptoms such as fatigue, weight gain, and depression.THRT is used to replace the thyroid hormone that's no longer being produced by the thyroid gland. THRT can help to alleviate symptoms such as fatigue, weight gain, and depression.
- Estrogen replacement therapy (ERT)
Medications
Medications such as levothyroxine can help to regulate thyroid hormone levels. Other medications, such as birth control pills, can help regulate estrogen and progesterone levels.
Here is a list of medications that can help with certain kinds of hormonal imbalance:
- Anti-androgen Medications
Anti-androgen medications block the effects of androgens (male hormones) in the body.
They are commonly used to treat the following conditions in individuals assigned female at birth:
- Hirsutism (excessive hair growth)
- Acne
- seborrhea (oily skin)
Some common anti-androgen medications include spironolactone, cyproterone acetate, and flutamide.
- Metformin
Metformin is a medication primarily used to treat type 2 diabetes. It works by decreasing the amount of glucose produced by the liver and increasing insulin sensitivity.
Metformin has also been used to treat polycystic ovary syndrome (PCOS) in individuals assigned female at birth.
- Flibanserin and Bremelanotide
These medications treat hypoactive sexual desire disorder (HSDD) in women.
Flibanserin works by increasing the levels of dopamine and norepinephrine and decreasing serotonin.
Meanwhile, bremelanotide increases the levels of melanocortins, increasing sexual desire.
- Eflornithine
Eflornithine is a medication used to reduce the growth of unwanted facial and chin hair in individuals assigned female at birth.
It works by inhibiting an enzyme called ornithine decarboxylase, which is involved in hair growth.
- Hormonal birth control
Hormonal contraception is a type of birth control that uses hormones to prevent pregnancy. There are several forms of hormonal birth control, including:
- Combined hormonal contraceptives
These contain estrogen and progestin and are available in oral pills, skin patches, vaginal rings, and injections. - Progestin-only contraceptives
These only contain progestin and are available as oral pills, injections, and implants.
Alternative therapies
Some alternative therapies like herbal supplements and acupuncture may help regulate hormone levels.
Surgery
In some cases, surgery may be needed to remove a tumor or other growth that is causing a hormonal imbalance.
It's important to note that the best treatment for hormonal imbalances will depend on the specific cause of the imbalance. A combination of treatments may be necessary to manage the symptoms effectively.
Additionally, a healthy lifestyle can help prevent and manage hormonal imbalances.
How Can I Get Rid Of Head And Neck Pain From Hormonal Imbalances?

Here are some self-care measures you can try at home to alleviate head and neck pain caused by hormonal imbalances. These can be very effective when they’re caused by menstruation or stress:
Relaxation techniques
A 2017 study mentions a strong link between stress and abnormal endocrine function. Deep breathing, yoga, or meditation can help reduce stress and tension in the head and neck.
According to one study, people who suffer from neck pain can greatly benefit from stress management and relaxation techniques. Even simply listening to your favorite song can help lower your stress levels. So keep your playlists on the ready!
Stretching and exercise
Gentle stretching and exercise can help improve blood flow and reduce muscle tension in the head and neck. It can also help regulate your appetite and hormone levels.
A 2017 study also shows that physical activity decreases insulin resistance. Insulin resistance may eventually lead to diseases like metabolic syndrome or type 2 diabetes. We can’t emphasize enough how important it is to get your body moving.
Hot and cold therapy
A heating pad or ice pack can help reduce pain and inflammation. You can check out our very own heating pad here.
Sleep hygiene
Practicing good sleep hygiene can improve sleep quality and alleviate symptoms of stress. This includes:
- Maintaining a regular sleep schedule
- Creating a comfortable sleep environment
- Avoiding screens before bedtime
It’s essential to avoid bright lights and screens before bedtime as these can affect your body clock. In a 2015 study, exposure to bright light before bedtime may stop the release of melatonin, the hormone responsible for sleep.
According to a study done in 2015, disrupted sleep can negatively impact your metabolism and the rhythm of hormone release. This can result in hormonal imbalances, obesity, diabetes, and improper appetite control.
Diet
Avoiding dietary triggers can reduce the likelihood of headaches and migraines. This can include:
- Caffeine
- Alcohol
- Processed foods
Eating a healthy diet rich in fruits, vegetables, and whole grains can also help to regulate hormone levels. These are very high in fiber which may help regulate certain hormones and help you maintain weight.
If you’re a woman, consider avoiding dairy products. In a 2017 study, dairy products were linked to decreased levels of female sex hormones.
Meanwhile, if you’re a man, you should consider avoiding alcohol. Alcohol may decrease your testosterone levels and may eventually lead to infertility.
Cigarette smoking may disrupt your endocrine function, increase cortisol, or alter the levels of thyroid hormones.
Hydration
Staying hydrated is important for overall health and may help prevent headaches and migraines.
Over-the-counter medications
You can also try taking Tylenol or Ibuprofen to relieve your headaches and neck pain quickly.
Takeaway
In a nutshell, hormonal imbalances can cause a lot of discomfort, especially in the form of neck pain and headaches. Hormones like estrogen, thyroid hormones, and cortisol can play a big role in causing these issues.
But don't worry. There are ways to alleviate the pain. Hormone replacement therapy, medication, and alternative therapies like massage and acupuncture can help. And remember the power of self-care - things like relaxation techniques, exercise, and a healthy diet can go a long way in managing symptoms.
If you're experiencing neck pain or headaches and think it might be related to hormonal imbalances, it's a good idea to chat with your doctor. They can help figure out the best course of action. Remember, you deserve to feel good, and there are plenty of options to help you get there!